Trauma and the Brain: Healing Techniques and Key Books to Guide Your Liberation by Katherine Kessler
Trauma can affect anyone, regardless of age or stage in life. From the innocent vulnerability of childhood to the complex challenges of adulthood, trauma – much like mental health stigma – knows no boundaries. It can be a silent intruder, reshaping how we think, feel, and interact with the world. At Scenic City Neurotherapy, we aim to change the conversation around mental health. Our mission is to help individuals understand that mental illness results from trauma or prolonged stress. These conditions are genuine brain health issues that can be treated and managed effectively. In this blog, we will explore:- The Impact of Trauma on the Brain
- Innovative Treatments for Mental Health:
- The Role of Personal Effort in Recovery
The Subtle Accumulation of Trauma
Trauma isn’t always a single, significant event. It can also stem from prolonged stress, such as relentless work pressure or more minor stressors that gradually wear down the brain. These seemingly “insignificant” stressors, when left unaddressed, can accumulate and contribute to the development of trauma in the brain. For example, consider the aftermath of a car accident. A minor collision may not seem significant on its own, but for someone already burdened with high-stress levels or past traumas, it can become a tipping point. Trauma often accumulates slowly, clouding thoughts, destabilizing emotions, and disrupting daily functioning. Understanding the intricate workings of our brain, as explored in Francine Shapiro’s “Getting Past Your Past: Take Control of Your Life with Self-Help Techniques from EMDR Therapy,” sheds light on how these seemingly minor stressors can profoundly impact our well-being.The Lasting Impact of Trauma on the Brain
Trauma, whether from a single event or prolonged exposure to distress, leaves a lasting imprint on the brain. It’s not just about emotional scars; trauma physically alters brain structures and functions, leading to mental illnesses such as PTSD, anxiety, and depression. When the brain experiences trauma, it can develop lesions or “dark spots,” disrupting communication within the brain. These lesions interfere with normal brain function, making it difficult for individuals to process emotions, think clearly, or respond appropriately to stress. This can manifest in various ways:- PTSD (Post-Traumatic Stress Disorder) is characterized by flashbacks, nightmares, and severe anxiety.
- Anxiety: Defined by persistent and excessive worry about various aspects of life.
- Depression: Described as a pervasive feeling of sadness, loss of interest in activities, and difficulty functioning daily.
The True Disease Behind Mental Health Conditions
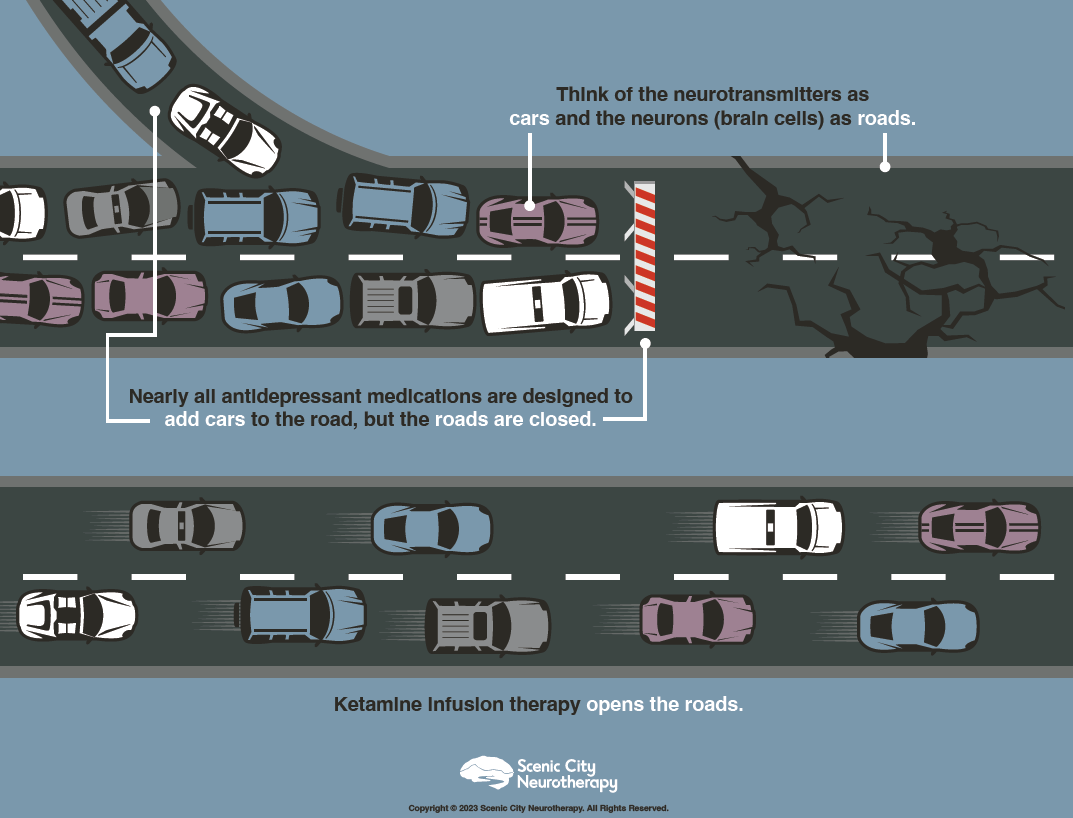
In his blog, “Treating the Symptoms vs. Treating the Disease,” MSKIT® expert Charles Miller highlights an essential misconception in psychiatry: the confusion of symptoms with the underlying disease. Think about this: what is the primary focus of psychiatrists’ treatment? You might quickly point to depression. However, this perception is rooted in an outdated theory known as the Serotonin Hypothesis. It’s crucial to acknowledge that depression is merely a symptom, not the underlying disorder itself. While psychiatrists traditionally prescribe medications to address symptoms such as depression, advancements in imaging technologies have significantly enhanced our understanding of how mental illness manifests within the brain. Depression is not the disease itself; instead, it’s a symptom indicating a more significant underlying issue. This primary issue, the root cause, lies in the breakdown of communication within the brain, manifesting as depression, anxiety, or PTSD. It’s clear that addressing this brain breakdown, stemming from prolonged stress or trauma, is essential for effectively treating mental illness. Unfortunately, antidepressants are unable to achieve this effectively. For years, antidepressants have targeted neurotransmitters, attempting to improve communication between brain cells. However, this approach has limitations because it does not repair the neuronal pathways the neurotransmitters must travel. Imagine neurotransmitters as cars and neuronal pathways as roads: just like adding cars to a closed road creates congestion, antidepressants attempt to increase neurotransmitter activity in obstructed pathways. To truly address the issue, we must first open these pathways, as illustrated below.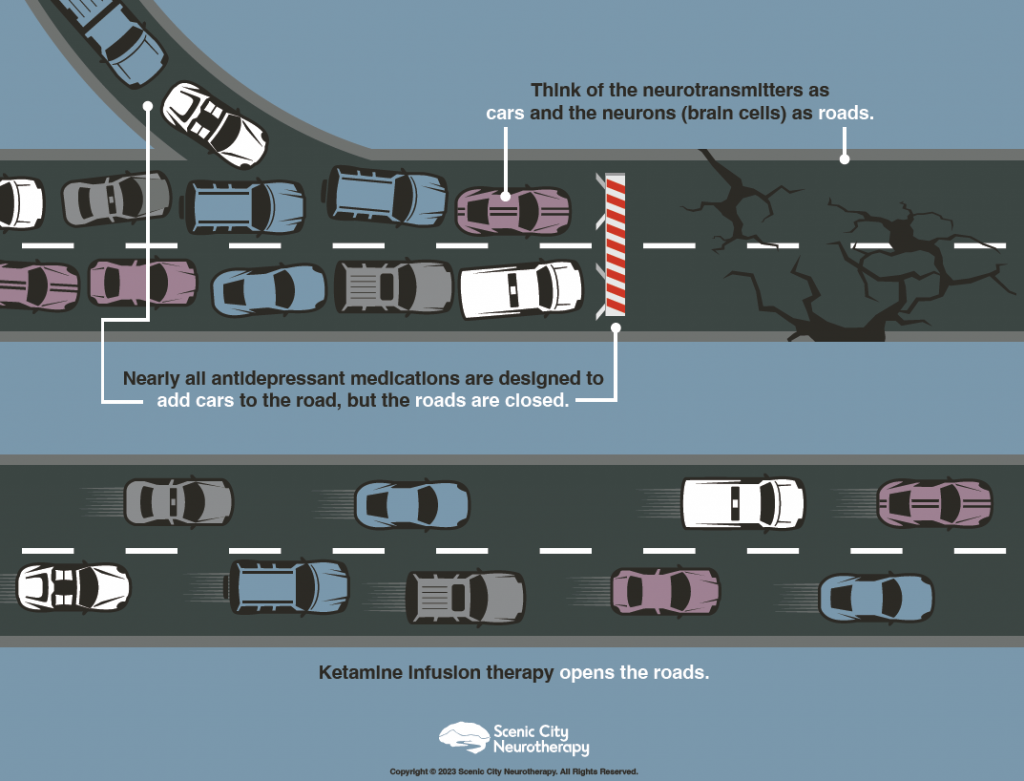
So, How Can We Open the Roads to Recovery?
Neurotherapies such as MSKIT® and TMS act as catalysts for brain healing. These therapies promote the growth of new neurons and repair damaged neurons, targeting the underlying causes of depressive symptoms. By doing so, they provide a genuinely effective approach to treating conditions previously deemed chronic and reliant solely on medication management.Revealing the Strength in the Limitations of Neurotherapy
Interestingly, the very limitation of these treatments is also their greatest asset. MSKIT® and TMS work by increasing brain-derived neurotrophic factor (BDNF) levels, a protein that plays a crucial role in neuroplasticity. As explained by Charles Miller:“BDNF is not just a support protein for neuron health. It is intricately linked to major brain functions and mood disorders, with direct implications for therapeutic interventions in psychiatry.”Neuroplasticity allows the brain to reorganize pathways, create new connections, and even create new neurons. It’s a natural process that helps us:
- Adjust to new experiences.
- Learn from our experiences.
- Integrate these experiences into our understanding of the future.
Neuroplasticity: Rewiring Minds, Transforming Lives
In my conversation with Charles Miller, he explained how understanding how neuroplasticity affects mood regulation and overall mental health can empower someone struggling to change their habits and actions. Neuroplasticity, the brain’s ability to change and adapt, operates by optimizing synaptic connections, where neurotransmitters like serotonin, dopamine, and norepinephrine are vital players. He said to think of it like this:“When your brain undergoes positive changes in areas rich in brain-derived neurotrophic factor (BDNF), such as the hippocampus and prefrontal cortex, your mood tends to improve, and you become more adaptable to stress. BDNF fosters the growth of new neurons and synapses, which is essential for overcoming mood disorders like depression. But neuroplasticity isn’t just about mood; it’s also about functionality and adaptation. When you face new challenges, your brain’s plastic nature allows it to refine neural pathways to better handle similar situations in the future. This adaptability isn’t just for short-term gains; it’s about long-term survival strategies. By enhancing your brain’s adaptability, you become better equipped to navigate life’s complexities and reduce emotional reactivity.”Understanding how your brain can change and adapt gives you the power to take control of your habits and actions. You can reshape your brain to support positive change and emotional well-being with effort and persistence. So, don’t be discouraged by setbacks; instead, see them as opportunities for your brain to learn and grow.
Putting New Connections to Use: The Work Ahead
While MSKIT® and TMS enhance neuroplasticity, providing the foundation for a better quality of life, the healing journey also requires active participation from the individual. The following books offer valuable insights and techniques for leveraging new neuronal connections. “The Body Keeps the Score” by Bessel van der Kolk Bessel van der Kolk, drawing on over thirty years of research and clinical practice, reveals how trauma reshapes the brain and body, leading to impaired emotional regulation, concentration, memory, trust, and comfort within one’s own body. This book teaches you how to regain control and harness your brain’s natural ability to heal, rebuilding the capacity to understand and feel your life’s experiences fully. “How to Do the Work” by Nicole LePera Dr. Nicole LePera’s book guides you toward a healthier, happier life by helping you break free from self-destructive patterns. Through her insights, you’ll better understand how childhood experiences impact your mental and physical health and uncover the root causes of your self-sabotaging behaviors. Dr. LePera then teaches you how to develop positive habits that enhance your well-being, empowering you to take control and improve your quality of life. “Getting Past Your Past” by Francine Shapiro Francine Shapiro’s book is best summarized by the Publisher: “Whether we’ve experienced small setbacks or major traumas, we are all influenced by memories and experiences we may not remember or don’t fully understand. ‘Getting Past Your Past offers practical procedures that demystify the human condition and empower listeners looking to achieve real change.” Francine Shapiro is the developer of EMDR (Eye Movement Desensitization and Reprocessing) therapy, a powerful technique for processing traumatic memories. You will learn actionable strategies that can complement professional therapy, aiding in resolving trauma-related symptoms. While this book provides valuable insights into the EMDR process, it is not a substitute for professional therapy. Bonus Read: “What My Bones Know” by Stephanie Foo Stephanie Foo wrote a beautiful memoir about her journey of healing from complex trauma. Her “What My Bones Know” narrative offers a powerful account of living with and overcoming trauma. Here’s an insightful excerpt from the book:“For the past two years, I had felt some form of shame whenever I was not in a state of blissed-out gratitude and appreciation. But Dr. Ham told me these negative emotions are not simply something to endure and erase. They are purposeful, beneficial. They tell us what we need. Anger inspires action. Sadness is necessary to process grief. Fear helps keep us safe. Completely eradicating these emotions is not just impossible; it’s unhealthy… True mental health looks like a balance of these good and bad feelings.”